There was a time in the not so distant past when medical claims processing was done in house.
This complicated and tedious task was often made the responsibility of doctors and physicians in addition to their interactions with the patients. These claims would need to be filled out by hand and then physically mailed to the insurance company before the doctor would be paid. Now, as Alleli Aspili of Health Works Collective points out, medical claims processors work to help physicians submit their claims and in turn get paid in a more efficient and timely manner.
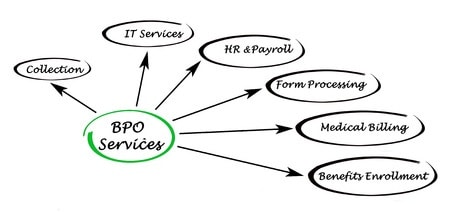
How does outsourcing medical claims processing run on a day to day basis?
The service provider receives high volumes of medical claims from the client which are then evaluated, coded and sent electronically to the appropriate insurance company. The insurance company then pays towards the balance provided by the physician in accordance with the terms of each individual policy. Since a significant amount of documentation is often required to make an insurance claim (patient information sheets, intake forms and proper services documentation) the task can be rather tedious and time consuming. This is where outsourcing firms become useful.
When electing to outsource medical claims processing to a third party provider, a physician not only frees up more of his or her own valuable time, but also places each of his patients’ claims in the hands of highly skilled and trained processors that can greatly reduce turnaround times.
This increased processing efficiency allows practices to see higher volumes of patients without the fear that uncompleted claims will pile up. Medical claims processors also use their expertise to resolve any issues that may arise during processing, avoiding any potential issues that the doctor may have run into had he or she processed the claim in house.
Third party outsourcing companies also have the advantage of using specialized software to speed up processing times while maintaining accuracy.
Ultimately, outsourcing medical claims processing leaves physicians with happier patients. The faster insurance claims are processed the more satisfied that patients will be with their visit overall. Patients also benefit from health care providers that are focused solely on their core competency of diagnosing and treating illness. The outsourcing of medical claims processing provides direct improvement in the quality health care that can be felt from the moment a patient walks through the door until the bills for the visit are paid. For this reason, the outsourcing of medical claims processing has become an industry standard today.
Telegenisys has been heavily involved in the outsourcing of medical claims processing since its inception over twenty years ago. During that time, we have gained valuable insights into the process that have led to increased efficiency and accuracy from processing agents. This blend of experience in the field and a talented workforce results in efficiency that saves our clients time and money. If your clinic or practice is in need of medical claims processing, please visit our website for a more detailed breakdown of our service offerings.









0 Comments